Suicide
Traumatic Brain Injury and Suicide
Concussions and skull fractures double the risk of death by suicide in a study.
Posted September 29, 2018

There’s a moment during an initial evaluation where you pull all the clues from a patient’s history and presentation together, and have, usually, a decent idea what is going on. Sometimes that moment comes pretty quickly, within minutes, when you see how someone interacts with you, family members, staff, taking into account the way they move and speak, how they think, what you know of their cultural norms. . . this is the “art” of psychiatry.
Long term sequelae of traumatic brain injury is one of those presentations that can be seen pretty quickly if you have the experience. Usually someone comes in complaining of poor concentration, often poor sleep, agitation and mood swings. They might have been diagnosed with bipolar disorder or attention deficit hyperactivity disorder. The medications didn’t work as expected…the stimulant made them more aggressive, the mood stabilizer at a normal dose made them very sleepy and out to lunch. The person tends to have a presentation subtly different from that of someone with ADHD. . . more word finding difficulties, noticeably more or unusually restricted emotional reactivity when talking about happy or sad events. Memory tends to be more of an issue.
Of course, the key to the history is the brain injury. Sometimes it’s obvious, like a car accident or a slip on the ice, and the symptoms never happened before then. Then there’s no mystery at all; it’s the more subtle forms that can surprise you. Kids who had a diagnosis of ADHD in childhood and got into football or soccer because it helped them get the extra energy out, and they had multiple concussions or headed the ball 10,000 times. Or maybe there was a bad car accident and the closed head injury was ignored because there were more severe, life-threatening injuries at the time. Poor sleep and moodiness could happen after a severe car accident whether the head was injured or not, after all.
Symptoms of traumatic brain injury in the short term include headache, sensory symptoms such as double vision or ringing in the ears, poor sleep or increased sleepiness, poor memory or memory loss. While there is generally improvement at first, longer term sequelae can include all of the above or a milder constellation of poor concentration, moodiness, poor sleep, and impulsivity. Turns out that the combination of moodiness and impulsivity has a cost when it comes to more serious issues such as all cause mortality and suicide.
A recent study of 7,418,391 people in Denmark over age 10 found that 7.6% had received medical care for a traumatic brain injury over a period of 34 years between 1980-2014. Some 34,500 or so people from this cohort died by suicide in this time period. A history of traumatic brain injury or skull fracture just about doubled the risk of suicide, and a history of severe traumatic brain injury increased the risk even higher. These results held even accounting for other factors, such as education, socioeconomic status, psychiatric disorders, marital status, sex, age, and more.
So what do we do about this problem? First, the best way to “treat” traumatic brain injury is to keep them from happening in the first place, or at least ameliorate them. Wear helmets when appropriate and use your seat belts. Don’t be too frisky in inappropriate shoes on the ice, as those slipping rotational injuries to the brain are terrible. If you do get a concussion, take it seriously. Follow medical advice, get plenty of rest, avoid watching movies, your phone or tablet screens, and everything else they tell you to do for a little while while your brain heals. If you have lingering symptoms, get more specialized help with speech or occupational therapists. I’ve seen people have improvement years after the fact.
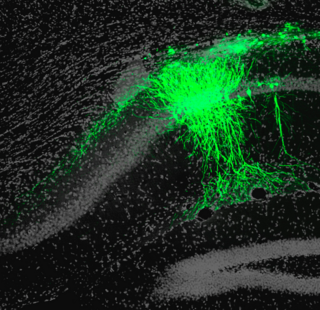
As my anatomy professor once said, the brain is the consistency of a fine custard. A brain injury rattles and breaks the delicate tree of axonal connections. The good news is the brain has some capacity to rewire itself, sometimes bypassing permanently broken areas, especially if you get proper treatment early on. Medication effects can be more unpredictable, but meds sometimes helpful, too, depending on the long lasting behavioral and cognitive effects of the injury.
As with any condition that increases risk of suicide, it’s important to educate yourself and your family. The most proven method of reducing suicide risk is reducing access to immediately lethal means, such as bridge barriers and removing access to firearms from someone who is at high risk. The national suicide prevention task force has an informative website at https://suicidepreventionlifeline.org and a 24 hour crisis line (1-800-273-8255). September is National Suicide Prevention Month.
Copyright Emily Deans, MD


