Depression
Stressed Out Physiology
Cool new findings about the stress response system and depression.
Posted January 31, 2019
All right folks, time to get basic with respect to hormones and the hypothalamic-pituitary-adrenal axis and mood disorders like depression. That means hunkering down and learning some physiology, because some really cool new insights come out of it.
Psychiatrists are used to thinking about the hypothalamic-pituitary-adrenal axis with respect to the very direct, relatively easily understood effects. The brain sends out signals to increase or decrease adrenaline and cortisol (steroids) from the adrenal glands that sit over the kidneys. Adrenaline and cortisol make you strong and awesome in the short term and tired and ragged and anxious when overused in the long term, which is a physiologic way of describing clinical depression and anxiety. As with every endocrine system, there are feedback loops that should work to turn off the system if it gets too revved up, but in clinical depression and anxiety, these feedback loops seem to fail. Too much cortisol long term without proper recovery leads to cortisol resistance in the brain, inflammation, and clinical depression and/or anxiety or other issues depending upon the vulnerability from your lifestyle and your genes.
But, psychiatrists, I have some news for you about the adrenals. There are several layers to those active little glands. One layer releases glucocorticoids, like cortisol, the stress hormone with which we are oh so familiar. The other releases mineralocorticoids, that have more to do with kidney regulation and blood pressure and stuff that I did my best to mostly forget about after my last exam about after residency ended. But the time to review is now.
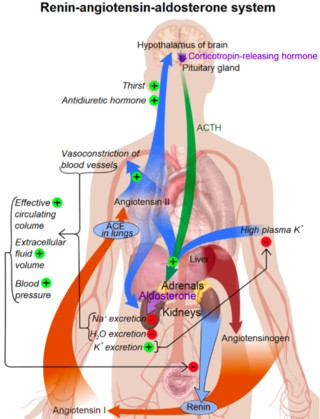
So. The kidneys, if you recall, release a little hormone called renin. It plays a pivotal role in modulating blood pressure. Renin cleaves angiotensinogen to make angiotensin I, which is made into angiotensin II (a little peptide that has a lot to do with increasing vasoconstriction and blood pressure) by a cool enzyme named ACE (angiotensin-I-converting enzyme). Here’s where we go from the kidney to the brain, because it turns out angiotensin II activates receptors in the brain that end up activating the release of cortisol. It’s all connected.
Even psychiatrists will remember a bit about this process, because a very popular type of blood pressure medication is called an ACE inhibitor. It is well-liked for being pretty effective, few side effects (outside an annoying cough), and for being protective of the kidneys in chronic diseases such as heart failure and diabetes. But here’s something you probably didn’t know about ACE inhibitors. Turns out that people on ACE inhibitors for blood pressure regulation have reduced risk of developing depression after starting the medication. Now this is observational data, but it is interesting and had a five year follow up of a thousand folks.
Take an ACE inhibitor, you reduce one of the pathways in the endocrine system that leads to the release of cortisol (when we know over-activation leads to cortisol resistance in the brain and symptoms of depression), and you tend to have less clinical depression over a long period of time. Seems straightforward enough.
Here is where things get pretty interesting. The angiotensin-converting enzyme, ACE, is produced by certain genes that have a number of polymorphisms in the population. That means, depending on your genes, your ACE will look and operate a little differently than someone else’s ACE. It turns out folks with certain genes for ACE have a higher incidence of depression than those with other genes. Specifically, people with the s4291 snp in the ACE gene have higher hypothalamic-pituitary-adrenal axis activity, hypercortisolism, and higher risk of developing major depressive disorder.
There are multiple alleles involved and it gets pretty confusing, but in general those genotypes with certain ACEs have higher cortisol response and a general hypercortisolism. These folks tend to have higher ACE concentrations and higher cortisol in the serum because the ACE is presumably less effective. And since everything is related, these same folks have higher risk of cardiovascular disease, which only makes sense.
So here is the big question. In folks with this genotype, do we try an ACE inhibitor as a treatment for depression? Other than observationally, this has never been studied, but it seems like a really important line of scientific reasoning to follow through. It’s a new topic of thought, but more papers are coming out.
Copyright Emily Deans MD


