I recently treated a lovely 45 year old female patient who had arrived in the ambulatory care department.
As I flicked through her triage notes in preparation for our consultation, it was apparent she had a “high stoma output”.
A stoma is a bag that attaches to the skin to act as a continuation of the gut – as the gut contents progress through the body, it reaches the stoma bag and is stored.
People have stomas when they have had operations on their digestive system, which may have occurred for a number of reasons including damage, infections, cancer and inflammatory bowel diseases.
Part 1: Admission
When a presentation like this occurs, doctors have to check several things. I ran through some of these points in my mind:
What is the reason for her stoma?
Why is she having high output?
Is this normal for her?
Is the stoma infected?
Is her stoma breaking down?
Does she need another operation?
Are there any complications of her high output?
Is she dehydrated?
Is she eating and drinking?
Does she have an infection elsewhere?
Are there consequences for her heart/lungs/liver/waterworks?
Are there dangerous changes to the salts in her blood?
Fortunately for my patient (and myself), the cause of her problem was simple.
She knew what was wrong.
She had experienced tingling and cramping of the muscles in her feet – she told me that her ‘magnesium and salts are low”.
She had a racing heart that had strong forceful beats – “I only get these when I know I’m dehydrated”.
We decided to top her up with fluid to bring her back to full hydration and to keep her in the department for an hour to monitor her recovery.
She had obviously had these problems before, which was confirmed when I scanned through her notes, finding that she must return regularly to this department for top ups of fluid. This phenomenon can be common in people with stomas, and other patients have shared similar experiences.
As the list above illustrates, however, problems with stomas can be much more complicated and dangerous. Although it was OK today, we must still be wary of what else could happen.
Is this bad? Why does this happen?
Workup
This lady had her entire large colon removed, which is a segment of the gut that helps absorb the water contained in the foods and drinks we consume.
This means that, unlike other people who are able to drink water to stay hydrated, normal oral intake is not adequate for this lady. Although she can absorb some liquid, it seems that she gradually becomes more and more depleted until she returns to be fixed at the hospital.
Fluid isn’t the only problem that the stoma has landed her with; food is another difficulty.
People with stomas are commonly recommended to avoid foods high in fibre and chewy foods such as red meat, to prevent obstruction of their gut, an essential organ made even more precious after its surgical shortening.
Compare this scenario to the outcome of eating these foods in a normal digestive system – fibre acts in the small bowel to slow down the digestion and absorption of food, while feeding the helpful bacteria found in the microbiome of the large bowel.
The ability to eat meat makes an adequate protein intake easy – maintaining nitrogen balance and providing the building blocks for muscle and immunity.
Moreso, these plant and animal foods are nutritious, providing us with the minerals, vitamins and other micronutrients needed for enzymatic processes and hormone production. A healthy gut is the best way to fuel our bodies for health; for my patient, these options are off the menu.
What can she eat?
Soft, fibreless foods. No fibrous vegetables, which removes many options. Limited meats. White bread. White pasta. What can she eat that fits the bill? She eats chips and crisps to get calories and salts, and drinks lucozade to maintain her electrolytes. This is not a balanced nor good diet for long term health.
I fear that the stoma is going to be a persistent reason for readmission for fluids. Her poor digestion will always throw her electrolytes out of balance. Finally, although it is easy for us to top up her fluids, we rarely provide broad spectrum micronutrient boosts via supplemental nutrition – With her chronic gut issues, it could be easy for her to slip into a deficiency of the micronutrients essential for normal workings of our physiology.
But why did the stoma happen?
This woman had presented a few years ago with a clot in her leg that had loosened to move up to her lung. This was a medical emergency (as a clot in the lung prevents breathing) and she was treated in hospital. By some unfortunate chance, a clot continued around her circulatory system and lodged itself in the blood supply to the gut. This rapidly halted the supply of oxygen and fuel to the gut, causing it to die. This lady now was a surgical emergency, requiring an operation to cut out her dead and damaged gut to prevent further serious problems; localised infection of the abdomen, leading to widespread infection of the blood, a procession potentially followed by death.
After she had the clot, she was placed on a blood thinning drug, warfarin, which she must take for the rest of her life. Warfarin is a blocker of vitamin K, which is a cofactor used to create the proteins that help normal clots formed. We find vitamin K in many foods, but a great source is in green leafy vegetables. To maximise the efficacy of the warfarin, this lady can no longer eat broccoli, kale and spinach because she is under instruction to reduce her vitamin K intake. Although she had to limit her intake of vegetables because of her stoma, her warfarin requirement adds another layer of restriction upon her intake of other micronutrients, too!
Why did the clot happen?
Who knows.
When we consider the sequaele of the clot, is that answer good enough?
What causes clots?
There are some serious causes that medical professionals look out for that are uncommon, such as inflammatory diseases, malignancy and inherited clotting diseases.
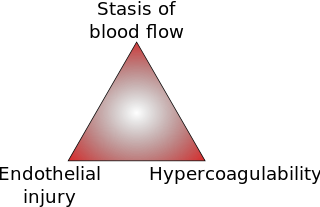
There are some common physiological contributors that tie into something called Virchow’s Triad – Inflammation, Hemodynamic changes and Endothelial Dysfunction.
Inflammation: A heightened state of the immune system to deal with insults and infection.
This can acutely occur with infection, trauma or exposure to an allergen. We’d expect this to be shown on a blood test via elevated C-Reactive Protein (CRP), increased numbers of ‘white’ immune cells, or other ‘acute phase proteins’ such as ferritin.
Furthermore, inflammation can be present at lower levels for a longer time. This might be produced by medical conditions such rheumatological or autoimmune diseases and can be monitored using CRP or the Erythrocyte Sedimentation Rate (ESR). However, as our appreciation of the influence of wider stimuli upon health increases, we may also see environmental and lifestyle factors contributing to inflammation. Chronic exposure to undesirable stimuli from the environment, food, or the gut (pollutants and chemicals, allergies or moulds, or dysfunctional compositions of gut flora, respectively), may cause the body to continually mount a low level inflammatory reaction.
Food is often spoken about as being pro- or anti-inflammatory. Anything that our body comes into contact to can be recognised by our immune system as something potentially harmful. Inflammatory foods are often associated as being the ones bad for our health – refined carbohydrates, trans-fatty acids, fried vegetable oils – with some dietary groups restricting food products from dairy to gluten to meat to green vegetables. We could also consider individual food sensitivities as contributors to inflammation. Each of these foods contain their own proteins and molecular identities so with respect to the state of each individual/group’s immune function, each food group may be the factor contributing to inflammation.
But what happens when the inflammatory process strikes?
If an individual reacts against common allergens, such as dairy, gluten or other proteins, the immune system is activated and acts locally, accessing affected areas by increasing blood flow and making tissue barriers more permeable. We see this as redness, heat, pain and swelling. However, we don’t see the wider effects of this reaction. This inflammatory response is produced by the release of immune mediators found throughout your body – If you have an infection in your finger, the blood from the top of your head to your furthermost toe will contain the same inflammatory signals – the inflammation is local, but the message is systemic.
Other environmental factors that provoke the immune system can be inflammatory – motor pollution, dust, pollen, chemicals in the water, drugs, pesticides, etc. What is important to understand is that although these are all individual factors, the response from the immune system is mediated by the same pathways and the same cells – the inflammatory response is simple and uniform. In this system, the inflammatory stimuli are funnelled into the same immune response.
Can the cumulative load of inflammatory stimuli contribute to a widespread increase in the activation of the immune system?
Can it contribute to an acute presentation of a clot in the leg?
What do you think?
As a side note, we have the ability to create anti-inflammatory substances that act on a system level. Both aerobic and resistance training (walking briskly or doing squats) provoke muscles to release ‘myokines’, that act to dampen down inflammation in the rest of the body.
Hemodynamic changes – stasis or turbulence.
At medical school, we are taught that common examples of stasis are sedentary behaviour, dehydration and smoking.
One cause of disruption is secondary to a clot, a product made more likely if the blood is hypercoaguable
There are wider determinants of hypercoaguability, such as when the proteins involved in the ‘Clotting Cascade’ are present at higher than normal levels. This is like filling water up behind a dam; the more water stored in the reservoir, the greater the catastrophe when the dam breaks. The more clotting factors you have stored away, waiting to get some action, the greater their effect will be when they are given the green light.
Factors that increase the quantity of clotting factors include low grade chronic inflammation, as mentioned above. Furthermore, a condition that affects a huge number of adults, Metabolic Syndrome, is implicated in hypercoagability. This syndrome is hypercholesterolaemia, hyperglycaemia, central obesity and hypertension. Otherwise known as having too much fat in your blood, too much sugar in your blood, such as in prediabetes/diabetes, a big tummy and high blood pressure. The metabolic syndrome is associated with
excessive levels of clotting factors, and the components of the syndrome play their individual roles – dysfunctional fat cells contribute to chronic inflammation, and hypertension is associated with endothelial dysfunction.
Endothelial dysfunction:
Endothelial cells line all of the blood vessels in the cardiovascular system. One of the simple roles of these cells is to provide a smooth surface to allow blood cells to flow efficiently, however, we are increasingly gaining an understanding of the complex roles of
endothelial cell function and dysfunction in health and disease. These cells control the responsiveness of the vessel to blood flow, widening and narrowing to control blood pressure. Hypertension, or high blood pressure, or inflammatory insults to the vessel wall, can upset the endothelial cells to alter their behaviour to become dysfunctional. When this occurs, these cells provide inflammatory environments for surrounding cells, increasing cell stickiness, increasing the recruitment of immune cells, provoking clot formation.
Discharge and Management Plan
This 45 year old woman had a clot in her leg, that migrated to her lungs, that migrated to her gut. An operation removed her gut and added a stoma. Her diet is further restricted by medication. She will reappear in the department and is booked for further fluids and electrolytes in the following weeks.
This lady may have been susceptible to acute insults such as being on a long-haul flight (sedentary) and dehydrated. These acute insults may have built upon a chronic inflammatory state – a low level inflammatory response to a food she is eating, a small smoking habit, lack of sunlight, lack of a varied intake of fruits and vegetables that provide electrolytes…
What lifestyle medicine could we prescribe to augment her pharmacological treatment?
Although this lady already has a stoma, she can still address the ‘pillars of lifestyle medicine’ to optimise her current health and prevent further deterioration – diet, physical activity, sleep, stress.
This lady needed a dietician review to address the difficulties she faces in maintaining proper nutrition due to her stoma and the conflict between nutrient dense vegetables and warfarin.
She would benefit from regular exercise such as walking regularly. As she increases her protein intake, she might feel like she is able to do some light ‘
resistance training’, such as walking up stairs or carrying bags. This is a good recommendation – improving blood flow, endothelial function, strengthening muscle, preventing falls, aiding metabolic health and benefiting body composition.
Putting an emphasis on sleep quality can improve her recovery and motivation in the daytime, while all of these factors in conjunction with stress management can modulate levels of inflammation.
Follow Up and Review
Blood clots in the leg, lung and gut are terrible problems to have. The sequelae of these events will be with this woman for the rest of her life.
Thanks for getting to the end of this blog. Before you go, answer these questions with this lady’s case in mind –
When does illness begin?
Does it take a trip to the ED with a blood clot to be ‘ill’?
What does “inflammation” mean to you?
Have you seen Virchow’s Triad anywhere else?